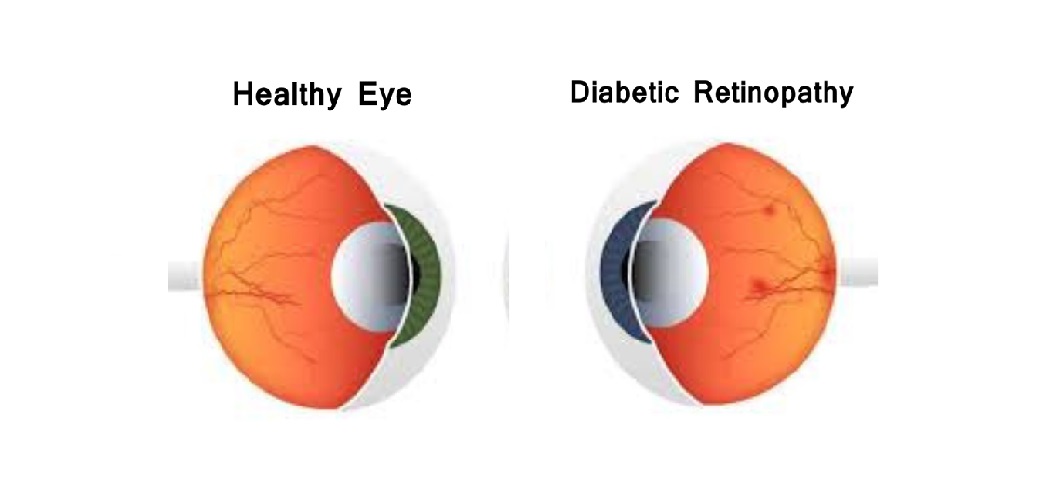
What is diabetic retinopathy?
Diabetic retinopathy is a serious eye condition that affects many people with diabetes. It occurs when high blood sugar levels cause damage to the tiny blood vessels in the retina. This damage can lead to vision problems and, if left untreated, blindness. These damaged blood vessels may start leaking fluid or bleeding, impacting vision. In the early stages of diabetic retinopathy, known as non-proliferative diabetic retinopathy, blood vessels may leak fluid, leading to macular edema and vision issues. In more advanced stages, known as proliferative diabetic retinopathy, abnormal blood vessels grow on the surface of the retina, potentially causing scar tissue, retinal detachment, and severe vision loss. Developing diabetes and maintaining high blood sugar levels can increase the risk of the condition. Managing diabetes through consistent monitoring of blood sugar levels, particularly hemoglobin A1c levels, is essential to reducing the risk of developing diabetic retinopathy. Developing diabetes and maintaining high blood sugar levels increase the risk of the condition, so regular eye exams are vital for early detection and monitoring.
What are the symptoms of diabetic retinopathy?
The symptoms of diabetic retinopathy can vary depending on the stage and progression of the condition. In the early stages, also known as non-proliferative diabetic retinopathy (NPDR), symptoms may be subtle or even nonexistent.
However, as the condition progresses, symptoms can become more noticeable and may include
- blurred or distorted vision,
- dark spots or floaters in the field of vision,
- difficulty seeing colors, and even vision loss or blind spots.
These symptoms can occur due to changes such as fluid leakage from small blood vessels, high blood pressure affecting the retina’s vessels, or the development of macular edema. As diabetic retinopathy advances to the proliferative stage, abnormal blood vessels may grow on the surface of the retina, leading to more severe symptoms. These symptoms can include sudden vision loss caused by bleeding into the eye (vitreous hemorrhage) or retinal detachment due to scar tissue. Regular eye examinations, including specialized tests like optical coherence tomography and fluorescein angiography, are crucial for early detection of these symptoms and effective management of the condition. Individuals with diabetes should closely monitor their vision and seek immediate medical attention if they notice any changes.
What are the treatment methods of diabetic retinopathy?
Treatment for diabetic retinopathy depends on the stage and severity of the condition. Laser treatment, also known as photocoagulation, can seal leaking fluid from blood vessels and prevent new blood vessels from growing. Injections of anti-VEGF drugs can help reduce swelling and slow the progression of the disease. In severe cases, vitrectomy surgery may be necessary to remove scar tissue and blood from the vitreous gel inside the eye. Managing blood sugar levels, high blood pressure, and cholesterol is also crucial for preventing the progression of diabetic retinopathy.
What happens if diabetic retinopathy is not treated?
If diabetic retinopathy is not treated, it can get worse and cause severe vision loss or blindness. Complications like macular edema can affect central vision, making it hard to read, recognize faces, or see details. Proliferative diabetic retinopathy can lead to bleeding in the eye due to abnormal blood vessel growth in the retina. If not treated, these new blood vessels can cause scar tissue and retinal detachment, leading to permanent vision loss. Untreated diabetic retinopathy can also increase the risk of developing glaucoma, which can damage the optic nerve. Regular eye exams are important for people with diabetes to catch diabetic retinopathy early. Managing diabetes by controlling blood sugar levels and high blood pressure can help prevent diabetic retinopathy from getting worse. Quick treatment is crucial to protect vision and quality of life.
Can diabetic retinopathy disappear?
While diabetic retinopathy cannot be completely cured, it can be managed effectively with treatment. Early detection and prompt treatment can slow the progression of the disease and preserve vision.
What are the 4 stages of diabetic retinopathy?
Diabetic retinopathy progresses through four stages: mild non-proliferative diabetic retinopathy, moderate non-proliferative diabetic retinopathy, severe non-proliferative diabetic retinopathy, and proliferative diabetic retinopathy.
What is the 4-2-1 rule in diabetic retinopathy?
The 4-2-1 rule in diabetic retinopathy is a guideline used by eye doctors to assess the severity of the condition and the risk of progression to proliferative diabetic retinopathy. It refers to four quadrants of the retina with severe retinal hemorrhages or microaneurysms, venous beading in two or more quadrants, and intraretinal microvascular abnormalities in at least one quadrant. If any of these criteria are met, the patient is at higher risk of developing proliferative diabetic retinopathy and should be monitored closely.
FAQ
Can you live a normal life with diabetic retinopathy?
Yes, you can live a normal life with diabetic retinopathy if you manage your diabetes effectively and receive appropriate treatment. Regular eye exams and prompt treatment can help preserve your vision and prevent complications.
Can I fly with diabetic retinopathy?
Flying with diabetic retinopathy is generally safe, but maintaining stable blood sugar levels and avoiding fluctuations in cabin pressure is essential. If you have severe retinopathy or other complications, consult your eye doctor before flying.
Does quitting sugar improve eyesight?
Quitting sugar may help improve blood sugar levels, which in turn can slow the progression of diabetic retinopathy. However, quitting sugar alone is not a guaranteed solution; managing overall blood sugar levels through a healthy diet, medication, and regular monitoring is more effective.
How long does it take for diabetes to damage the eyes?
The time it takes for diabetes to damage the eyes varies depending on how well blood sugar levels are managed. Diabetic retinopathy can develop within a few years if blood sugar levels remain consistently high. Early signs may appear within five years of diagnosis, but it may take longer for some individuals. Regular eye exams are essential for detecting early signs of eye damage and managing complications. Effective blood sugar and blood pressure control can help delay the onset of diabetic retinopathy and prevent vision loss.
Can I exercise with diabetic retinopathy?
Yes, you can exercise with diabetic retinopathy, but consult your doctor to ensure you’re doing so safely. Exercise can help manage blood sugar levels, but avoid high-intensity or high-impact activities that may increase the risk of retinal damage.
Which exercises should diabetic patients avoid due to retinopathy?
Diabetic patients with retinopathy should avoid exercises that involve heavy lifting, straining, or sudden head movements. These activities can increase eye pressure and the risk of retinal bleeding or detachment. Always consult your doctor for specific recommendations.
Our Bestsellers
Categories
Company
Media
Follow Us
© Copyright Biotech /Terms Of Use - Privacy Policy
Version 2_CT_1212222