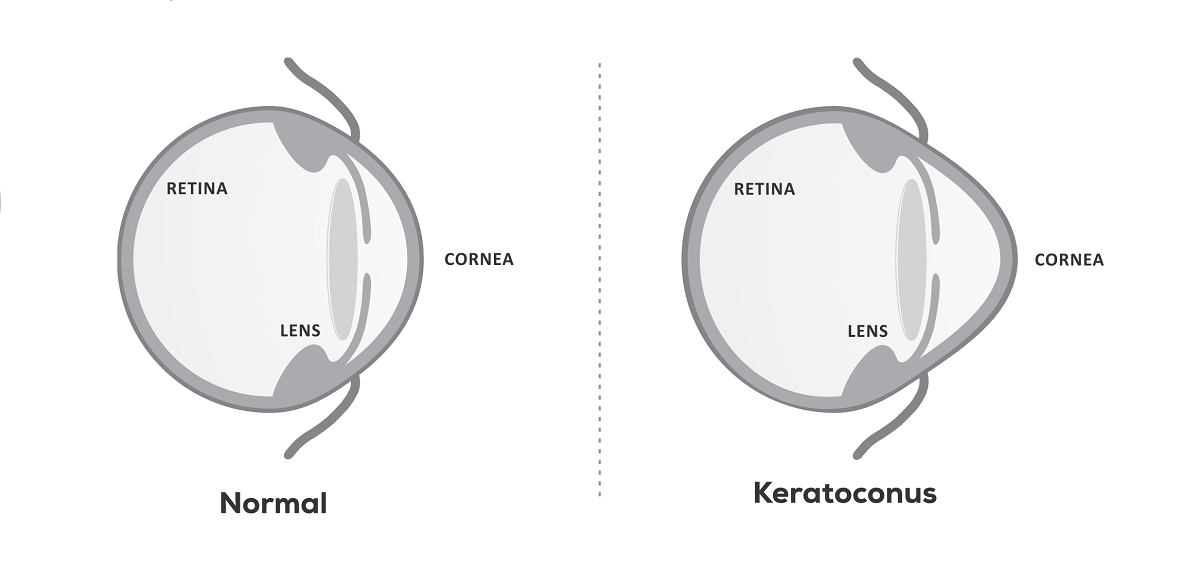
What is Keratoconus and How Does It Occur
Keratoconus is a disorder of the eye characterized by the progressive thinning and bulging of the cornea. The cornea, which is typically round in shape, becomes cone-shaped in people with keratoconus. This abnormal shape disrupts the normal refraction of light entering the eye, resulting in distorted vision. The exact cause of keratoconus is not fully understood, but it is believed to involve a combination of genetic predisposition, environmental factors such as UV light exposure, and inflammatory processes.
The cornea’s structural integrity relies on collagen fibers, which provide strength and support. In keratoconus, these collagen fibers become weakened, leading to progressive thinning and bulging of the cornea. Over time, the cornea loses its smooth, regular curvature, resulting in irregular astigmatism and blurred vision.
What are the Symptoms of Keratoconus?
Symptoms of keratoconus include
- blurred or distorted vision,
- increased sensitivity to light (photophobia),
- frequent changes in eyeglass or contact lens prescriptions,
- difficulty with night vision, and seeing halos around lights.
As the condition progresses, people with keratoconus may experience eye strain, frequent eye rubbing, and sudden changes in vision clarity. It’s essential for individuals experiencing these symptoms to seek evaluation by an eye care professional for proper diagnosis and management.
How is Keratoconus Diagnosed?
Diagnosing keratoconus involves a comprehensive eye examination by an eye doctor or ophthalmologist. This examination may include tests such as corneal topography, which maps the shape of the cornea, and slit-lamp examination to assess the integrity of the corneal tissue. Additionally, measuring corneal thickness (pachymetry) and assessing visual acuity are common diagnostic procedures to confirm the presence and severity of keratoconus
Which Age Groups Does Keratoconus Affect?
Keratoconus can affect individuals of all ages, but it most commonly develops during adolescence or early adulthood. However, the onset and progression of the disease can vary widely among affected individuals. In some cases, keratoconus may stabilize or progress slowly over many years, while in others, it may progress more rapidly, leading to significant visual impairment.
Is Keratoconus Genetic?
There is evidence to suggest that keratoconus may have a genetic component, as it often runs in families. Individuals with a family history of keratoconus may have an increased risk of developing the condition themselves. However, the inheritance pattern of keratoconus is complex, and multiple genetic and environmental factors may contribute to its development.
Does Keratoconus Require the Use of Glasses or Lenses?
In the early stages of keratoconus, vision correction with eyeglasses or soft contact lenses may be sufficient to manage symptoms and improve visual acuity. However, as the condition progresses and corneal irregularities become more pronounced, gas permeable contact lenses may be recommended to provide better visual correction and stability. Gas permeable lenses can help to vault over the irregular corneal surface, providing a more uniform refractive surface for clearer vision.
Can Keratoconus Be Treated Surgically?
Yes, keratoconus can be treated surgically in cases where other interventions such as contact lenses are insufficient to manage symptoms or improve vision. Surgical options for keratoconus include corneal collagen cross-linking, Intacs and corneal transplantation.
What Options Are Available for Keratoconus Treatment?
Treatment options for keratoconus include eyeglasses or contact lenses to correct vision, corneal collagen cross-linking which involves the use of UV light and riboflavin (vitamin B2) to strengthen the cornea and halt progression, Intacs implants to reshape the cornea, and corneal transplant surgery for advanced cases of keratoconus.
How Does Keratoconus Treatment Work?
Keratoconus treatment aims to address the progressive thinning and bulging of the cornea, which characterizes this condition. One of the primary treatment approaches is corneal collagen cross-linking, a procedure designed to strengthen the corneal tissue and halt the progression of keratoconus. During corneal collagen cross-linking, riboflavin (vitamin B2) eye drops are applied to the cornea, followed by exposure to ultraviolet (UV) light. This process induces cross-linking of collagen fibers within the cornea, increasing its stiffness and stability over time. Corneal collagen cross-linking helps to prevent further deformation of the cornea and preserve visual acuity, particularly in the early stages of keratoconus.
In addition to corneal collagen cross-linking, corrective measures such as glasses or contact lenses may be prescribed to improve visual clarity and correct refractive errors associated with keratoconus. Specialized contact lenses, including rigid gas permeable lenses or scleral lenses, are often recommended to provide better visual correction and improve the shape of the cornea. In cases where keratoconus has progressed to a more advanced stage and vision cannot be adequately corrected with conservative measures, surgical interventions such as Intacs implantation or corneal transplantation may be considered.
Intacs are small plastic rings inserted into the cornea to flatten its curvature and improve visual function. They provide structural support to the cornea, reducing irregular astigmatism and enhancing visual acuity.
Corneal transplantation, either penetrating keratoplasty or lamellar keratoplasty, involves replacing the damaged portion of the cornea with healthy donor tissue obtained from a donor. This surgical procedure is reserved for people with advanced keratoconus who have not responded to other treatment modalities. Overall, the goal of keratoconus treatment is to stabilize the cornea, improve visual function, and optimize the quality of life for affected individuals.
How Long Does Keratoconus Treatment Take?
The duration of keratoconus treatment varies depending on the specific interventions and the individual’s response to treatment. Corneal collagen cross linking, a common treatment for keratoconus, typically takes about one to two hours per eye. During the procedure, riboflavin (vitamin B2) eye drops are applied to the cornea, followed by exposure to ultraviolet (UV) light. Recovery from corneal collagen cross-linking may take several days to weeks, during which patients may experience temporary discomfort and sensitivity to light.For other treatments such as Intacs implantation or corneal transplantation, the duration can vary significantly based on factors such as the complexity of the procedure, the patient’s overall health, and the extent of corneal damage. Intacs implantation surgery usually takes about 30 to 60 minutes per eye, while corneal transplantation may take longer, often requiring several hours for the procedure itself, along with a period of post-operative recovery.
What is the Recovery Process After Keratoconus Treatment?
The recovery process after keratoconus treatment varies depending on the specific intervention and individual factors. After corneal collagen cross-linking, patients may experience temporary discomfort, light sensitivity, and blurry vision, which typically resolve within a few days to weeks. During this time, it’s essential to avoid rubbing the eyes and follow post-operative instructions provided by the eye care provider. After Intacs implantation or corneal transplantation, patients may require a longer recovery period, including follow-up appointments to monitor healing and assess visual acuity.
Our Bestsellers
Categories
Company
Media
Follow Us
© Copyright Biotech /Terms Of Use - Privacy Policy
Version 2_CT_1212222